Americans miss almost 113 million days of work each year due to migraine attacks. For those actively seeking treatment, prescription drugs, injections and other invasive methods only add to the stress and misery of the condition.
With no known cause, migraneurs are often forced to travel a long and winding road with endless challenges before maybe stumbling upon a treatment that offers some degree of reprieve. But as migraine awareness improves, so do options for care.
New technology and research has revealed a revolutionary treatment option with promising results that don’t include the side effects of numbing medications. Known as Neurostimulation Therapy, tests suggest that this method of treatment has helped to reduce or eliminate symptoms in over 80% of patients where other forms of treatment have failed. Here’s what you should know:
What is neurostimulation therapy?
Neurostimulation therapy involves a minimally invasive surgical procedure that uses light electrical currents to incite the nerves associated with delivering pain signals to the brain. The procedure involves four parts:
- Neurostimulator – a device that generates the electrical currents or pulses.
- Leads – tiny bundles of wire that deliver the pulses to targeted nerves.
- Controller – for patients to turn treatment on or off and adjust stimulation levels.
- Programmer – for physicians to adjust and refine stimulation programs.
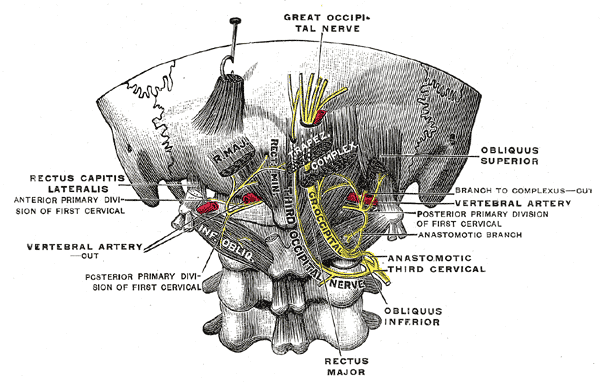
For migraine relief, these leads are placed beneath the skin near the occipital nerves using a very minimal surgical procedure. The actual neurostimulator device is also implanted, often around the abdomen or buttock area. A physician will program the device to cater to the patient’s specific needs and patients can turn the device on or off and control intensity levels using their own remote.
How does it work?
The occipital nerves are believed to be a major conductor of pain signals between the brain and body. Neurostimulation therapy provokes the nerves in this region using light electrode pulses to block pain signals that want to communicate with the brain. This significantly or completely dissolves the experience of pain and replaces it with a tingling sensation.
Statistics
In 2013, St. Jude Medical, a global medical device company, conducted the first large-scale study of neurostimulation therapy and chronic migraines. 15 medical centers throughout the country were involved in the study, which tested 157 participants who suffered an average of 21 migraine attacks each month. After twelve weeks of neurostimulation therapy, the following conclusions were reported:
- 65% of patients described their pain relief as ‘excellent’ or ‘good’.
- 88% said they would recommend neurostimulation therapy to a friend.
- 68% of patients experience an improvement in their quality of life.
- 67% expressed being ‘satisfied’ or ‘very satisfied’ with the results.
The Journal of Head and Face Pain also summarized that preliminary reports suggest 60% to 80% of patients with chronic migraine symptoms who did not find relief with medical intervention responded to neurostimulation.
A number of additional studies exist that display promising statistics on behalf of neurostimulation therapy for migraine pain and further research is being conducted to better understand the effects of this treatment on other types of chronic pain.
Side Effects
Overall, neurostimulation therapy reduces pain with fewer side effects than medication or injections. However, because neurostimulation therapy is a relatively new treatment, physicians are uncertain about the existence of long-term effects. Current risks include:
- Infection at implant site
- Fluid leakage
- Nerve damage
- Lead movement (which can disrupt treatment)
- Post-surgery pain
- Skin irritation on electrode site.
- Nausea or dizziness
- Isolated instances of lung atelectasis, seizures, pain, paresthesias and edema.
Am I a Candidate?
Individuals who qualify for neurostimulation therapy procedures fit the following profile:
- Have been clinically diagnosed with chronic migraine syndrome.
- Possess a strong belief that migraines are chronic (lasting more than 4 hours at a time and occurring at least 15 days per month).
- Are considering alternative treatments, like surgical intervention.
- Have been to the emergency room for migraine pain.
- Have tried daily over the counter or prescription migraine medication with little or no improvement.
- Have tried other forms of therapy like injections, chiropractic therapy or acupuncture with little or no improvement.
Talk to your doctor to find out if neurostimulation therapy is right for you. A thorough analysis of your medical and treatment history will indicate whether you might be a good candidate for alternative care options like this. Keeping a migraine diary that outlines your experience with treatments and therapies will greatly help to determine if neurostimulation therapy will have a positive influence on your quality of life. If you qualify, most procedures offer a non-surgical trial period with the device so that it’s effects can be test driven before implantation.